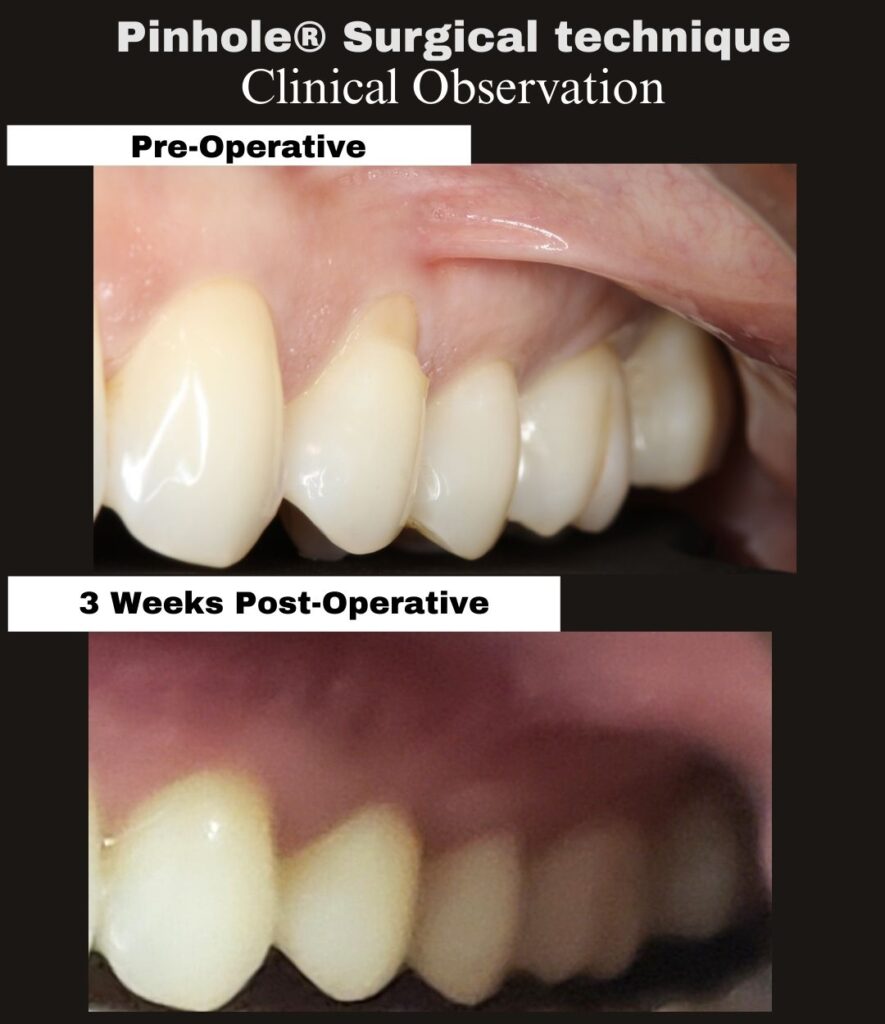
This entry documents a post-operative day 1 clinical observation following treatment of gingival recession at teeth #20–21 using the Pinhole® Surgical Technique.
Case Identification
• Procedure date: 02/09/26
• Post-operative interval: 1 day (02/10/26)
• Procedure time: 11:41 AM – 1:01 PM (80 minutes)
• Tooth/Teeth: #20–21
At this acute interval, the treated site demonstrates expected early-phase edema and localized erythema with maintained soft-tissue positioning. Final gingival margin position has not yet declared, as continued biologic remodeling is expected during maturation.
The Pinhole® Surgical Technique was developed by Dr. John Chao as a biologically guided, minimally invasive approach to the management of gingival recession.